 This question comes up a lot, and as more variations of each practice continually emerge, it becomes increasingly difficult to answer..... A SIMPLE, one line answer (at the risk of overgeneralization) that many have used….acupuncture is aimed at the treatment of disease states and pain through insertion of needling specific points on the body’s surface with the intention of changing a person’s energy flow (or Qi), whereas dry needling aims to make changes to the target tissue by inserting needles specifically into that tissue. Over time, the practices have started to gravitate toward similarity, as various forms of acupuncture have become more westernized and dry needling has incorporated more eastern thinking. There are many forms of acupuncture practiced globally, although historians trace all roots back to China, with acupuncture documented as early as the second century. Like any practice, it has evolved over the years, but those rooted in traditional Chinese medicine are most familiar to people in the western world. One example of the latter..some dry needling approaches teach using alcohol swabs on the skin prior to treatment, whereas others have adopted the eastern thinking that swabbing the skin with alcohol might could kill “good” bacteria. More on the fundamental differences: One tenet of Traditional Chinese Medicine is that many conditions in the body result from disruptions to balance of qi, which is literally translated as “vital force.” Acupuncture emerged and continues to this day as one approach to restore body balance through realignment of qi. By strategically placing needles into acupressure points along meridians (or channels), through which qi is thought to flow, acupuncture will restore the balance of qi and manage pain or whatever other symptoms are being targeted. Dry needling, sometimes referred to as trigger point dry needling, has traditionally been based on inserting needles to disrupt trigger points, which we could define as taut, localized ischemic bands. In layman’s terms, think of a “knot” in the muscle with limited blood flow. As dry needling has evolved, we’ve begun to appreciate more global effects of DN beyond simply breaking up these trigger points. When we stick a needle in the body, the effects are felt throughout many systems, not simply in the soft tissue it physically contacts. Uses basically the same needles. They might differ in the specifics of which needles are used more often though. Needles can vary in length and texture, with different needle qualities having both plusses and minuses. Generally speaking, you’ll see acupuncture using more needles and keeping them in for longer. It is not uncommon for needles to remain 20-30 minutes, or even longer. Many DN approaches practice a more “get in, get out” strategy; going directly for a trigger point with one or a few needles and then removing it when the acute twitch response has subsided, whereas acupuncture does not seek to make changes to tissue. But again, more and more dry needling approaches are teaching longer insertion durations as the role of the nervous system (not simply the target tissue) gains greater acceptance. Neurophysiological considerations…while we know from ultrasound imagery that the insertion of a needle into the body causes some disruption to the body’s structure, modern thinking in the dry needling world also appreciates how this process can also have profound effects throughout the nervous system as a whole, from the release of chemicals known to decrease pain sensitivity. Generally, DN inserts the needles deeper than acupuncture because the target tissue often lies far beneath the surface; there are some techniques even specifically targeted to “peck” the bone. Both can be paired with electrical stimulation for an added treatment effect. One criticism that has been leveled at dry needling from the alternative medicine community has been that dry needling as practiced by physical therapists is “only taught in weekend courses.” This critique represents a very superficial understanding of the educational pathway. Physical therapy education, which is now exclusively delivered at the doctoral level in the United States, includes intensive lab-based instruction in anatomy and physiology (again, at the doctoral level). Many physical therapy programs share the EXACT same anatomy lab facilities as MD/DO programs housed at the same institution. For additional reading see, Notes from Structure and Function Dry Needling course Allan Phillips, PT, DPT Ventana Physiotherapy Oro Valley, Arizona History of Graston Technique… David Graston was competitive water skier; sustained injury but frustrated with poor results from other treatments; went and used jar top as a self massage tool and improved; used his engineering knowledge to create specialized instruments, hence the birth of Graston Technique
More than just scraping and making the skin red (people often associate Graston with these giant bruises, but contemporary thinking has evolved quite significantly).. Many variables to consider for best possible treatment…size of instrument, which treatment edge, shape of body part being treated, speed of stroke, length of stroke, type of stroke, target tissue length, angle of instrument edge, treatment duration… I did go in without an intention of purchasing the instruments….but I ended up getting them anyway (in full disclosure, the military and student discounts did play a role in my decision to ultimately purchase) Stuff I liked…
What is plantar fasciitis (“PF”)? If you’ve had it, you certainly know it doesn’t feel very good! “Plantar fasciitis” is very broad term commonly applied to any pain on the bottom of the foot. Sometimes the condition is not plantar fasciitis at all, but instead a strained foot muscle or “fat pad syndrome” (more on that diagnosis later). Ultimately, for the patient, the specific diagnosis doesn’t matter too much because the treatment approach will be very similar (assuming we stay in the realm of orthopedics and aren’t dealing with a condition unrelated to muscles, tendons/ligaments or bones).
I call plantar fasciitis an “equal opportunity offender” because you’ll find it in elite athletes who dedicate insane training volumes to their sport but also in sedentary people who walk no further than the bathroom, and of course every type of person in between. In other words, you can get it from doing too much or from not doing enough. Practically speaking, you’ll find plantar fasciitis manifested in several different ways. First, the classic presentation of plantar fasciitis is isolated tenderness toward the front/middle of the heel, at a landmark called the medial calcaneal tubercle. Although the pain might extend along the entire foot, for this version of plantar fasciitis, the hallmark is localized pain at that specific point on the heel. Additionally, patients with this presentation will often feel pain at its worst in the first step of the morning. Another similar common presentation is pain further back toward the heel but still on the bottom of the foot over a broader area. This is sometimes called fat pad syndrome if the primary source of pain is the fat pad on the heel rather than the plantar fascia. But again, the causes behind the condition are very similar so the treatment approach should look similar as well. Plantar fasciitis may also refer to pain in the arch of the foot. Again, this may be a result of true plantar fascia inflammation or it could be referred pain patterns from elsewhere in the body. It could also be a strained muscle, as there are many muscles on the bottom of the foot that perform a variety of functions. 1. CHANGE YOUR CADENCE Changing to a faster cadence is one way to decrease stress on the foot. Cadence is a more complicated issue than footstrikes-per-minute, but do know that changing to a faster cadence is often accompanied by OTHER changes known to decrease loading, most notably a forward lean and shift to a more forefoot strike. My personal preference is that if you are going to change mechanics, let the mechanical changes emerge as a BYPRODUCT of focusing on cadence rather than flooding your mind with technical cues that may be difficult to implement in real time. 2. FIND SOFT RUNNING SURFACES This isn’t possible 100pct of the time for everyone, but the sacrifice can be worth it. When I’ve been on the cusp of injury, I’ve done endless loops around a grass soccer field to get the mileage in while minimizing the risk of further injury. There’s precedent for this too at the highest levels of running, as USA Olympians Galen Rupp and Dathan Ritzenheim (both historically injury prone) have been known to do up to 20 miles around a 600m grass loop! As a caveat, there isn’t as much evidence to support this strategy as we might think. That said, anecdotally countless runners report fresh and rejuvenated legs after dedicating the time and effort to run more on grass. Article: The Benefits of Running on Grass (Triathlete Magazine) 3. TRAIN SMART! Probably the most important strategy of all. Smart training provides the right amount of stimulus for the body to adapt and become stronger; excess training provides a stimulus too great for the body’s adaptive capabilities. This doesn’t necessarily mean physical breakdown though. Pain could be a warning signal, especially notable given the high density of nerve tissue in the feet. With excess loading, the foot can become more sensitive to pain, meaning it takes less of a stimulus to provoke a higher level of pain than before. All this information returns us to the concept that the first line of defense against plantar fasciitis (or any injury for that matter) is to pick the right training loads. 4. SELF-MASSAGE YOUR FOOT For self-massage, the simplest would be direct pressure. Just put your finger on a tender spot and hold it there. You can also massage along the foot, finding those “rough” spots or knotted areas and working them out. Though people often report mixed results from self-massage in other areas of the body, the foot tends to respond quite well, perhaps because the foot is so dense with nerve tissue. Another form of self-massage is instrument assisted soft tissue mobilization. This is just a fancy term for using different objects to perform self-massage! There are plenty of commercial products on the market, some designed specifically for the feet. Everyone has their own preferences, from the hardness of a golf ball to the softness of the spikey ball. Of all the implements available the spikey ball seems to be the most well received. Every is likely aware of the conventional advice to treat shin splints: R.I.C.E., stretching, a switch to softer running surfaces, training plan modifications, maybe a new pair of shoes or a change in running technique. While each of these techniques have merit as treatment approaches, sometimes you need to think a little outside stay on your feet with minimal disruption in training.
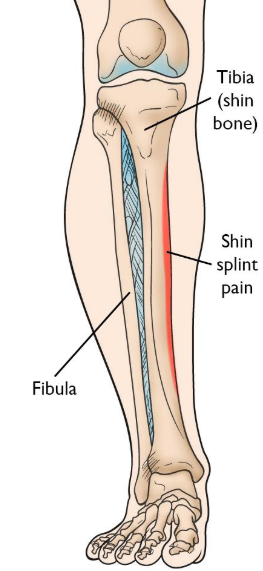
Now, before we treat "shin splints" it is important to confirm that shin splits are really what we're dealing with. For purposes of this article, we'll associate the term shin splints the diagnosis of medial tibial stress syndrome ("MTSS"). In the popular lexicon, shin splints are frequently associated with a myriad of diagnoses including anterior compartment syndrome, anterior tibial tendonitis and stress fractures or stress reactions, among others. The shin splints we'll discuss here involve pain along the inside of the shin as shown below. Do you need an elbow brace or strap to help you get through your regular pickleball games? What if I told you there’s a BETTER way to manage your elbow pain AND prevent it from coming back? If you’re willing to devote ten minutes per day to a few exercises and some self-massage techniques, there’s a good chance you can ditch that elbow strap and get back to the court WITHOUT pain and with improved motion in your arm to have you playing at the top of your game?
If you’re having pain on the outside of your elbow, there’s a good chance you could have lateral epicondylitis, or more commonly known as “tennis elbow.” This condition can also occupational, such as with people who turn a wrench for a living or perform any task involving repetitive twisting of the forearm. I even have seen a pastor with this condition, which he attributed to doing some renovations around his church (talk about hands on!) He was actually a pretty decent golfer too (though not playing frequently at the time) which may have irritated the area previously. Here are four simple do-it-yourself interventions plus one simple treatment that work quite reliably when done consistently. If these approaches don’t resolve your pain AND help you return to the pickleball court, the next step would be to seek help from a rehab professional who has other techniques available and can also look for potential causes such as in shoulder function. Mobilization with movement – Whether performed on yourself or delivered by a professional, this is the “go-to” technique for persistent tennis elbow. Both options are shown below. Note that you can vary the angle of arm bend to provide different stimuli to the area, as patients can vary in which angle works best for them. Typically the treatment is performed by applying lateral pressure and then having the patient grip and release, though you’ll find different variations on the same theme commonly practiced. The key point here is that PAIN SHOULD REDUCE with this treatment. If pain is getting worse, this likely isn’t the right treatment for you. Which is fine, because there are other options…. |
AuthorAllan Phillips, PT, DPT is owner of Ventana Physiotherapy Archives
December 2023
Categories
All
|
2951 N. Swan Rd.
Suite 101, inside Bodywork at Onyx
Tucson, Arizona 85712
Call or Text: (520) 306-8093
[email protected]
Terms of Service (here)
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Proudly powered by Weebly


 RSS Feed
RSS Feed