|
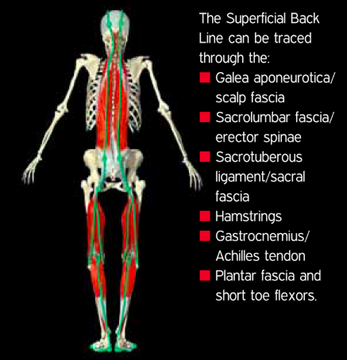
What is plantar fasciitis (“PF”)? If you’ve had it, you certainly know it doesn’t feel very good! “Plantar fasciitis” is very broad term commonly applied to any pain on the bottom of the foot. Sometimes the condition is not plantar fasciitis at all, but instead a strained foot muscle or “fat pad syndrome” (more on that diagnosis later). Ultimately, for the patient, the specific diagnosis doesn’t matter too much because the treatment approach will be very similar (assuming we stay in the realm of orthopedics and aren’t dealing with a condition unrelated to muscles, tendons/ligaments or bones). I call plantar fasciitis an “equal opportunity offender” because you’ll find it in elite athletes who dedicate insane training volumes to their sport but also in sedentary people who walk no further than the bathroom, and of course every type of person in between. In other words, you can get it from doing too much or from not doing enough. Practically speaking, you’ll find plantar fasciitis manifested in several different ways. First, the classic presentation of plantar fasciitis is isolated tenderness toward the front/middle of the heel, at a landmark called the medial calcaneal tubercle. Although the pain might extend along the entire foot, for this version of plantar fasciitis, the hallmark is localized pain at that specific point on the heel. Additionally, patients with this presentation will often feel pain at its worst in the first step of the morning. Another similar common presentation is pain further back toward the heel but still on the bottom of the foot over a broader area. This is sometimes called fat pad syndrome if the primary source of pain is the fat pad on the heel rather than the plantar fascia. But again, the causes behind the condition are very similar so the treatment approach should look similar as well. Plantar fasciitis may also refer to pain in the arch of the foot. Again, this may be a result of true plantar fascia inflammation or it could be referred pain patterns from elsewhere in the body. It could also be a strained muscle, as there are many muscles on the bottom of the foot that perform a variety of functions. 1. CHANGE YOUR CADENCE Changing to a faster cadence is one way to decrease stress on the foot. Cadence is a more complicated issue than footstrikes-per-minute, but do know that changing to a faster cadence is often accompanied by OTHER changes known to decrease loading, most notably a forward lean and shift to a more forefoot strike. My personal preference is that if you are going to change mechanics, let the mechanical changes emerge as a BYPRODUCT of focusing on cadence rather than flooding your mind with technical cues that may be difficult to implement in real time. 2. FIND SOFT RUNNING SURFACES This isn’t possible 100pct of the time for everyone, but the sacrifice can be worth it. When I’ve been on the cusp of injury, I’ve done endless loops around a grass soccer field to get the mileage in while minimizing the risk of further injury. There’s precedent for this too at the highest levels of running, as USA Olympians Galen Rupp and Dathan Ritzenheim (both historically injury prone) have been known to do up to 20 miles around a 600m grass loop! As a caveat, there isn’t as much evidence to support this strategy as we might think. That said, anecdotally countless runners report fresh and rejuvenated legs after dedicating the time and effort to run more on grass. Article: The Benefits of Running on Grass (Triathlete Magazine) 3. TRAIN SMART! Probably the most important strategy of all. Smart training provides the right amount of stimulus for the body to adapt and become stronger; excess training provides a stimulus too great for the body’s adaptive capabilities. This doesn’t necessarily mean physical breakdown though. Pain could be a warning signal, especially notable given the high density of nerve tissue in the feet. With excess loading, the foot can become more sensitive to pain, meaning it takes less of a stimulus to provoke a higher level of pain than before. All this information returns us to the concept that the first line of defense against plantar fasciitis (or any injury for that matter) is to pick the right training loads. 4. SELF-MASSAGE YOUR FOOT For self-massage, the simplest would be direct pressure. Just put your finger on a tender spot and hold it there. You can also massage along the foot, finding those “rough” spots or knotted areas and working them out. Though people often report mixed results from self-massage in other areas of the body, the foot tends to respond quite well, perhaps because the foot is so dense with nerve tissue. Another form of self-massage is instrument assisted soft tissue mobilization. This is just a fancy term for using different objects to perform self-massage! There are plenty of commercial products on the market, some designed specifically for the feet. Everyone has their own preferences, from the hardness of a golf ball to the softness of the spikey ball. Of all the implements available the spikey ball seems to be the most well received. Also note the “classic” PF treatment, which is the frozen water bottle. Stick a water bottle in the freezer until the contents turn to a block of ice. Then remove the bottle from the freezer and use it as a massage roller for the bottom of your foot. Finally, when treating the foot, understand that it is extraordinarily difficult to preferentially target the plantar fascia. When we treat the soft tissues of the feet we’re hitting many different structures and layers. One tip is to work in gradually, regardless of what type you are doing. There are many layers to the foot tissues. Going in with an aggressive pressure can neglect the topmost layers, which might be where the problems are. 5. WORK THE CALVES The foot itself is not the only area that we need to address. The calf muscles are one place to start away from the foot, and some may suggest starting there even BEFORE the foot. As with the foot, I recommend starting with some type of soft tissue treatment such as self-massage most commonly with a foam roller or stick. The plantar fascia is contiguous with fascia running all along the back side of our bodies. For active people pushing off and landing repeatedly, the calf muscles are responsible for propulsion and deceleration, putting them under demand with nearly step taken. In less active people, the calf muscles can become what we’d call adaptively shortened. As an extreme example, think of high heels. Those shorten the muscles in the back of the lower leg (the calves) if worn for prolonged periods of time. This should be fairly easy to envision, which is why I am focusing on the extreme. 6. WORK THE TOES Toe spreading is another exercise to help the muscles of the foot. It seems really simple, but it can be a challenge to hold this even for a healthy foot. If you can’t get the muscles to spread your toes, you can use your hand to manually do it first. Especially check the flexibility of the BIG TOE. It should be able to extend to at least and 80 to 90 degree angle, which would be having the toe point almost directly skyward. A stiff big toe could result from tight tissue or a joint restriction and is often overlooked in the assessment of foot and lower leg function. 7. DO RUNNING DRILLS For runners, probably the most neglected area of returning to activity after PF is making the TRANSITION from walking to running. The foot might feel great doing exercises and walking but the loading increase from walking to running (to even faster running) can be extreme. It is probably one of the most frustrating things of rehabbing PF. Many people have stories of taking weeks off only to feel their pain return to its original intensity during the first run back. But fear not…this doesn’t have to be you!! If you haven’t done running drills since you were a kid, don’t feel embarrassed at first. This is a judgment free zone!! My key drills are the low skip, high skip, bounding, backward skipping. You can get very complex with your drill progressions but for the purpose of reconditioning the foot after a bout of PF, we’re simply trying to recondition the tissues and more importantly, the nervous system, for the demands of constant landing.
8. CROSS TRAIN This is generally not something that resolves with rest alone. I know the frustration of saying, “I’ll just take a week off” only to experience knife-like pain in the first few steps running again. For that reason, unless walking itself is excruciatingly painful, our goal is to provide a maximum opportunity for recuperation with the minimal intrusion on the training or activity levels. If possible, it is best to maintain some activity, but make sure you work around, not into pain. For cardio in general, the rule of “does it hurt?” applies. If something reproduces or causes severe pain, then you probably shouldn’t do it. Water running, swimming and the rowing machine are typically non-painful options to maintain fitness when dealing with foot pain. Cycling and the elliptical are perfectly fine if they don’t cause pain, but they can put slightly more strain on the back of the legs if there’s significant tightness in your calves or hamstrings. --- Want help implementing any of these strategies or looking for hands on treatment to help you resolve your foot pain and resume training? Reach out to us through the website or email. Allan Phillips, PT, DPT Physical Therapy in Oro Valley and Tucson
0 Comments
Leave a Reply. |
AuthorAllan Phillips, PT, DPT is owner of Ventana Physiotherapy Archives
December 2023
Categories
All
|
2951 N. Swan Rd.
Suite 101, inside Bodywork at Onyx
Tucson, Arizona 85712
Call or Text: (520) 306-8093
[email protected]
Terms of Service (here)
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Proudly powered by Weebly

 RSS Feed
RSS Feed