|
“Shin splints” is one of those broad terms that many people (doctors included) use to describe a very wide range of conditions. In other words, if someone says “shin splints” what they actually mean can be several different things.
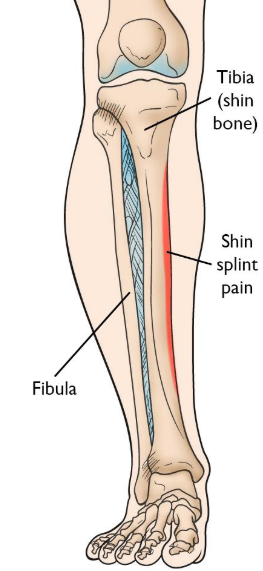
Going “by the book,” shins splints is synonymous with “medial tibial stress syndrome” which is basically irritation at the connection between muscle (usually the posterior tibialis) and the tibia (shin bone). Tends to be a repetitive strain condition, but can have underlying causes in mechanics, strength, mobility or training load; or in the case of bone injuries there can be nutrition causes as well. Occasionally, the irritation might be on the muscle itself without any irritation to the bone, in which case it would be some form of posterior tibialis strain or tendinopathy of the posterior tibialis tendon, if closer to the ankle. As for bone injuries, we can have a stress reaction or a stress fracture. The difference is these is basically one of degree. Think of a stress reaction as the beginnings of a stress fracture. Whereas a stress reaction might dissipate within days if given time to heal, a full blown stress fracture can know you out of a solid couple of months. The hallmark sign will be pain/tenderness in a specific spot, whereas many other shin conditions will display pain along a longer segment. On the outside of the shin on the more “meaty” muscle side, we can have anterior tibial tendinopathy or tibialis anterior strain. You may also hear the term “compartment syndrome” which gets tossed around quite liberally referring to pain on the outside of the shin, but full blown compartment syndrome is a true medical emergency, where you’ll experience numbness, loss of circulation and changes to skin texture. The gold standard to diagnose compartment syndrome is to measure the pressure inside the compartment. Sometimes, shin pain isn’t shin pain at all, but is instead nerve pain from the lower back. You could also experience nerve-like symptoms from irritation at the outside of the knee. But in these scenarios, the symptoms are less likely to be associated with movements or direct stress to the lower leg. High ankle sprain is also slim possibility, but unless you’ve had an acute incident of twisting your ankle or lower leg, it’s safe to rule this one out. Ultimately, these diagnoses are simply descriptive labels. Most important is identifying how and why these are happening, but understanding that many different conditions can exist under the realm of “shin splints” is a good way to start!
0 Comments
Every is likely aware of the conventional advice to treat shin splints: R.I.C.E., stretching, a switch to softer running surfaces, training plan modifications, maybe a new pair of shoes or a change in running technique. While each of these techniques have merit as treatment approaches, sometimes you need to think a little outside stay on your feet with minimal disruption in training.
Now, before we treat "shin splints" it is important to confirm that shin splits are really what we're dealing with. For purposes of this article, we'll associate the term shin splints the diagnosis of medial tibial stress syndrome ("MTSS"). In the popular lexicon, shin splints are frequently associated with a myriad of diagnoses including anterior compartment syndrome, anterior tibial tendonitis and stress fractures or stress reactions, among others. The shin splints we'll discuss here involve pain along the inside of the shin as shown below. |
AuthorAllan Phillips, PT, DPT is owner of Ventana Physiotherapy Archives
December 2023
Categories
All
|
2951 N. Swan Rd.
Suite 101, inside Bodywork at Onyx
Tucson, Arizona 85712
Call or Text: (520) 306-8093
[email protected]
Terms of Service (here)
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Proudly powered by Weebly

 RSS Feed
RSS Feed