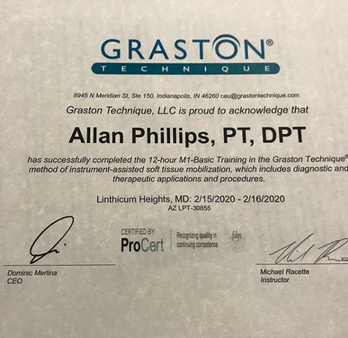
 This question comes up a lot, and as more variations of each practice continually emerge, it becomes increasingly difficult to answer..... A SIMPLE, one line answer (at the risk of overgeneralization) that many have used….acupuncture is aimed at the treatment of disease states and pain through insertion of needling specific points on the body’s surface with the intention of changing a person’s energy flow (or Qi), whereas dry needling aims to make changes to the target tissue by inserting needles specifically into that tissue. Over time, the practices have started to gravitate toward similarity, as various forms of acupuncture have become more westernized and dry needling has incorporated more eastern thinking. There are many forms of acupuncture practiced globally, although historians trace all roots back to China, with acupuncture documented as early as the second century. Like any practice, it has evolved over the years, but those rooted in traditional Chinese medicine are most familiar to people in the western world. One example of the latter..some dry needling approaches teach using alcohol swabs on the skin prior to treatment, whereas others have adopted the eastern thinking that swabbing the skin with alcohol might could kill “good” bacteria. More on the fundamental differences: One tenet of Traditional Chinese Medicine is that many conditions in the body result from disruptions to balance of qi, which is literally translated as “vital force.” Acupuncture emerged and continues to this day as one approach to restore body balance through realignment of qi. By strategically placing needles into acupressure points along meridians (or channels), through which qi is thought to flow, acupuncture will restore the balance of qi and manage pain or whatever other symptoms are being targeted. Dry needling, sometimes referred to as trigger point dry needling, has traditionally been based on inserting needles to disrupt trigger points, which we could define as taut, localized ischemic bands. In layman’s terms, think of a “knot” in the muscle with limited blood flow. As dry needling has evolved, we’ve begun to appreciate more global effects of DN beyond simply breaking up these trigger points. When we stick a needle in the body, the effects are felt throughout many systems, not simply in the soft tissue it physically contacts. Uses basically the same needles. They might differ in the specifics of which needles are used more often though. Needles can vary in length and texture, with different needle qualities having both plusses and minuses. Generally speaking, you’ll see acupuncture using more needles and keeping them in for longer. It is not uncommon for needles to remain 20-30 minutes, or even longer. Many DN approaches practice a more “get in, get out” strategy; going directly for a trigger point with one or a few needles and then removing it when the acute twitch response has subsided, whereas acupuncture does not seek to make changes to tissue. But again, more and more dry needling approaches are teaching longer insertion durations as the role of the nervous system (not simply the target tissue) gains greater acceptance. Neurophysiological considerations…while we know from ultrasound imagery that the insertion of a needle into the body causes some disruption to the body’s structure, modern thinking in the dry needling world also appreciates how this process can also have profound effects throughout the nervous system as a whole, from the release of chemicals known to decrease pain sensitivity. Generally, DN inserts the needles deeper than acupuncture because the target tissue often lies far beneath the surface; there are some techniques even specifically targeted to “peck” the bone. Both can be paired with electrical stimulation for an added treatment effect. One criticism that has been leveled at dry needling from the alternative medicine community has been that dry needling as practiced by physical therapists is “only taught in weekend courses.” This critique represents a very superficial understanding of the educational pathway. Physical therapy education, which is now exclusively delivered at the doctoral level in the United States, includes intensive lab-based instruction in anatomy and physiology (again, at the doctoral level). Many physical therapy programs share the EXACT same anatomy lab facilities as MD/DO programs housed at the same institution. For additional reading see, Notes from Structure and Function Dry Needling course Allan Phillips, PT, DPT Ventana Physiotherapy Oro Valley, Arizona
0 Comments
Bottom line: If you have an injured limb and are unable to train as normal (or train at all), training the other side can still yield benefits of the injured side Question time….Let’s say you injure your left knee. What is the best strategy for your training plan? 1 Push through pain no matter how bad it is. Don’t change your training plan. Rest is for sissies 2 Continue to train the right knee, so long as it doesn’t further injure or provoke symptoms in the left 3 Stop training both legs because you don’t want you’re right leg to become too strong relative to your left and develop an asymmetry There is a “best” answer here and that answer is number 2. Answer number 1 is ridiculous, so we’ll put that one aside. Number 3 sounds compelling and while it wouldn’t necessarily be “wrong” to go that direction, there are several reasons why number 2 is better. Again, this is all based on the caveat that the training you do for the uninjured limb doesn’t put the injured limb at further risk of injury or delay healing. For example, let’s say you were doing some single leg activities on the uninjured leg, but each impact sent a “shock” through the injured leg. Your best bet is to either find different activities or delay training the uninjured limb until it can be done safely without provoking the injured limb. In the literature, the concept of training effects on one limb being felt on the opposite side limb is called cross education. And to the surprise of some, the evidence is quite clear that cross-education works. Unfortunately, what should be the standard of care (training the rest of the body at the highest level possible in a way that supports the healing process), is instead a novel concept to many. There are several reasons why cross-limb education is not promoted more. One is that the medical process is often siloed and sees the world with tunnel vision. For example, most orthopedic surgeons are going to just look at the injury and not even consider. That’s not meant to be critical, it’s just the nature of their job. They’re good at going into a damaged body part and making structural corrections using surgical techniques. They aren’t paid to tell you how to train. Similarly, most PT’s in a “traditional” outpatient setting aren’t getting paid to consider the opposite leg (and in some cases are actively discouraged from looking anyplace other than the site of the injury…Not their fault, that’s just the nature of the system in which they work). uninjured limb.
What does the evidence say?....A meta-analysis by Green (2018) reviewed 96 studies on cross education involving healthy young adults, healthy older adults and patients, finding an average strength gain via cross education of 18% in young adults, 15% in older adults, and 29% in a patient population. Although prior meta analyses had shown conflicting results on gender differences and upper versus lower limb effects, the studies compiled by in the Green meta-analysis revealed no significant differences. Overall, the average cross body transfer ranged from 48%-77% in the compiled studies, meaning that the immobilized limb experienced strength gains of 48%-77% of the trained limb. Again, this isn’t just one study on a homogenous group of subjects…this is 96 studies in a variety of populations. (Another interesting finding was that electrically stimulation of muscles appeared to have a greater cross-education effect than voluntary stimulation). WHY cross education works remains up for debate but most evidence points to neurological mechanisms as the primary factors. Per Cirer-Sastre (2017), “this owes to the fact that no significant vascular adaptations have been found, nor were any histological changes in hypertrophy levels, in enzyme concentration, in contractile protein composition alteration, in fiber type or in cross-sectional area.” In short, strength is function of the nervous system, and the effects of nervous system output are global, meaning not specific to any single body part. Although the evidence has been relatively settled that cross-education does exist via single sided training, HOW to facilitate cross-education is less clear although a meta-analysis of ten studies by Cirer-Sastre, “to optimize contralateral strength improvements, cross-training sessions should involve fast eccentric sets with moderate volumes and rest intervals. Finally, approaching this from a pragmatic standpoint, if you sustain an injury to a limb, you could continue training the other limbs and have three “good” limbs or you could stop training both the injured and non-injured arm/leg and have two “good” limbs. Which sounds better? The concern about developing asymmetries is logical, but overall is far overblown. As we know from the research, the cross-education effect will mitigate strength losses from inactivity by an injured limb. Further, even if cross-education did not exist, you’re better off having to bring one limb up to speed rather than losing strength in both sides have having two limbs to return to normal. Simply makes no sense why you would voluntarily weaken a perfectly healthy limb. Even if an asymmetry develops during a recovery period, its not as though you were going to hop right back into peak training after you get over the injury. You might as well give yourself the highest “baseline” with a strong, healthy limb rather than let both sides regress. REFERENCES Lara A. Green & David A. Gabriel (2018) The effect of unilateral training on contralateral limb strength in young, older, and patient populations: a meta-analysis of cross education, Physical Therapy Reviews, 23:4-5, 238-249, DOI: 10.1080/10833196.2018.1499272 Cirer-Sastre R, Beltrán-Garrido JV, Corbi F. Contralateral Effects After Unilateral Strength Training: A Meta-Analysis Comparing Training Loads. J Sports Sci Med. 2017;16(2):180–186. Published 2017 Jun 1. History of Graston Technique… David Graston was competitive water skier; sustained injury but frustrated with poor results from other treatments; went and used jar top as a self massage tool and improved; used his engineering knowledge to create specialized instruments, hence the birth of Graston Technique
More than just scraping and making the skin red (people often associate Graston with these giant bruises, but contemporary thinking has evolved quite significantly).. Many variables to consider for best possible treatment…size of instrument, which treatment edge, shape of body part being treated, speed of stroke, length of stroke, type of stroke, target tissue length, angle of instrument edge, treatment duration… I did go in without an intention of purchasing the instruments….but I ended up getting them anyway (in full disclosure, the military and student discounts did play a role in my decision to ultimately purchase) I know the feeling. Been running along and then BAM…who just whacked the side of my knee with a baseball bat?? Oh, wait…there’s no one around…
Knee pain is one of the classic issues that can befuddle runners. The problem is that not all knee pain is created equal. Saying “knee pain” can mean any number of things, and quite often the problem is far away from the knee. Sure, we need to calm down the pain if we want to start moving normally, but long-term progress requires us to search a little deeper. The purpose of this guide is to help you as an athlete navigate what can seem like an unsolvable puzzle, especially when you’ve been trying to find a solution for weeks, months or even years. |
AuthorAllan Phillips, PT, DPT is owner of Ventana Physiotherapy Archives
December 2023
Categories
All
|
2951 N. Swan Rd.
Suite 101, inside Bodywork at Onyx
Tucson, Arizona 85712
Call or Text: (520) 306-8093
[email protected]
Terms of Service (here)
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Privacy Policy (here)
Medical disclaimer: All information on this website is intended for instruction and informational purposes only. The authors are not responsible for any harm or injury that may result. Significant injury risk is possible if you do not follow due diligence and seek suitable professional advice about your injury. No guarantees of specific results are expressly made or implied on this website.
Proudly powered by Weebly

 RSS Feed
RSS Feed